What to know
This clinician brief describes properties and sources of polychlorinated biphenyls (PCBs), routes of exposure, populations at risk, health effects, and clinical evaluation, management, and counseling of patients.

Properties
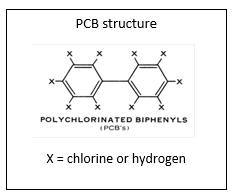
Polychlorinated biphenyls (PCBs) are a family of manufactured chemicals that were used in multiple industrial and commercial applications because of their insulating and nonflammable properties. Production of PCBs was banned in the United States in 1979 when their ability to accumulate in the environment and to cause harmful health effects became known.
Commercial PCB products were mixtures of different PCB congeners and contained small amounts of polychlorinated dibenzo-p-dioxins (PCDDs or dioxins) and polychlorinated dibenzofurans (PCDFs). These contaminants generally had greater toxicity than the PCBs themselves, although some PCBs also demonstrate dioxin-like toxicity.
Sources
Although PCBs are no longer commercially produced in the United States, occupational exposure may occur among workers who repair or perform maintenance on old electrical equipment, demolish old buildings containing PCBs, or handle materials at hazardous waste sites.
PCBs have been used in products such as the following:
- Electric transformers and capacitors
- Heat exchange and dielectric fluids
- Diffusion pump oils
- Flame retardants
- Hydraulic and lubricating fluids
- Plasticizers
- Paints
- Caulking compounds
- Adhesives
- Pesticide extenders
- Inks and carbonless transfer paper
PCBs are resistant to biodegradation and tend to persist in the environment for months to years. These compounds are highly lipophilic, allowing strong adsorption to soil and sediments. Once released into the environment, PCBs biomagnify upward through the food chain in aquatic organisms. Cycling of PCBs within the ecosystem occurs with volatilization from land and water surfaces into the atmosphere, followed by wet or dry deposition, and subsequent revolatilization (ATSDR, 2000 & 2011; Gouin et al., 2004; Hansen, 1999; Wania and & Mackay, 1996).
Routes of Exposure
Ingestion. The main route of exposure to PCBs in the general population is the consumption of contaminated foods, particularly fish, meat, dairy, and poultry, although PCB concentrations in food have decreased over time. Potentially high exposures may occur in recreational and subsistence anglers who consume fish from local contaminated waters.
PCBs readily cross the placenta during pregnancy and accumulate in breast milk. In-utero and breastfeeding exposure may occur in children of PCB-exposed mothers who frequently eat contaminated fish. Fetuses and neonates are potentially more sensitive to PCBs than adults because their immature enzyme systems may not metabolize and excrete PCBs efficiently and because of their rapidly developing tissues and organ systems.
Infants can be exposed to PCBs via ingestion of breast milk (Ando et al. 1985; Jacobson et al. 1984a; McLachlan 1993). However, given the scientific understanding at this time, the benefits of breastfeeding outweigh any potential risks of PCB exposure through breast milk (ATSDR 2000). With numerous protective health benefits, breast milk continues to be the ideal nutrition for infants. In nearly every circumstance, the Centers for Disease Control and Prevention and the American Academy of Pediatrics recommend that nursing individuals continue to breastfeed their babies despite the potential presence of environmental contaminants (AAP, 2019; ATSDR, 2021).
Children consume a greater amount of food per kilogram of body weight compared to adults. Therefore, they may have proportionally greater exposure to PCBs compared to adults when eating food with the same level of PCB contamination.
Dust and other PCB-containing residue from paints, caulk, and other materials in old buildings can be ingested (Grimm et al., 2015). Children may be especially susceptible, as they play on the floor and put their hands inside their mouths often.
Inhalation. Inhalational exposures to PCBs are primarily occupational (Bosetti et al., 2003). Although PCBs evaporate slowly at room temperature, volatility increases as these substances are heated. Vaporization of PCBs from old electrical equipment that overheats may result in significant inhalational exposure. Old buildings constructed or renovated between 1950 and 1979 may contain PCBs in caulk, paints, adhesives, fireproofing materials, ceiling tiles, and fluorescent light ballasts. Inhalation of PCB-containing dust in these older buildings may be another source of indoor exposure (Grimm et al., 2015).
Children may be more vulnerable to developing adverse health effects than adults due to physiologic differences such as having a higher minute ventilation (amount of air inhaled or exhaled per minute) compared to adults. Behavior including crawling and playing on the floor closer to PCB-containing dusts may also place children at increased risk for exposure.
Dermal. PCBs can be absorbed through the skin following contact with contaminated equipment, water, or soil. Most dermal exposures are occupational (Bosetti et al., 2003).
Populations at Risk
PCB exposure and risk of associated adverse health effects may be potential concerns for the following patients:
- Workers in occupations with risk of PCB exposure
- Repair or maintenance of electrical transformers, capacitors, cables, or other older equipment
- Disposal of PCB containing materials at hazardous waste sites
- Firefighting and other emergency response
- Semiconductor and related industries
- Plumbing and pipefitting
- Metal finishing, electroplating
- Waste oil processing
- Manufacture of timber products
- Medical laboratory technician/technologist
- Paving and roofing
- Noncellulose fiber industry
- Repair or maintenance of electrical transformers, capacitors, cables, or other older equipment
- People who consume fish from waters contaminated with PCBs
- Sport anglers and subsistence fishers, many of whom are American Indian/Alaska Native, ethnic minorities, and immigrant populations
- Children of mothers who frequently ate contaminated fish or wild game before or during pregnancy
- Sport anglers and subsistence fishers, many of whom are American Indian/Alaska Native, ethnic minorities, and immigrant populations
- People living near incinerators, PCB disposal facilities, Environmental Protection Agency (EPA) National Priorities List (Superfund) sites, municipal landfills, poorly maintained toxic waste sites, or areas where illegal or improper dumping of waste containing PCB may have occurred
- People exposed through inhalation to smoke and soot from transformer or capacitor fires
- Farming families who consume food produced from their own farm-raised beef and dairy cattle
- Many farms in the Midwest United States in the 1940s and 1950s had concrete silos coated with sealants containing PCBs. These materials peeled off over time and were mixed with silage used to feed beef and dairy cattle. Although most of these silos have been dismantled and removed, some older silos remaining are a potential PCB source (Hansen, 1987; Humphrey, 1983; Schantz et al., 1994).
- Many farms in the Midwest United States in the 1940s and 1950s had concrete silos coated with sealants containing PCBs. These materials peeled off over time and were mixed with silage used to feed beef and dairy cattle. Although most of these silos have been dismantled and removed, some older silos remaining are a potential PCB source (Hansen, 1987; Humphrey, 1983; Schantz et al., 1994).
- People who spend prolonged periods of time in buildings containing old construction materials with PCBs, including children who attend schools built between 1950-1980 (Dai et al., 2016).
Health Effects
Exposure to PCBs has been associated with adverse health effects in humans. The risk of adverse health effects varies depending on exposure dose, exposure concentration, timing, frequency, duration, and a patient's personal characteristics. Most environmental exposures are difficult to quantify in terms of dose, frequency, and duration.
Specific PCB congeners are categorized into groups and may be associated with different health effects, and people are typically exposed to complex mixtures containing multiple congeners (Wolff and Taniolo, 1995). These mixtures may also be contaminated with other substances such as dioxins and dibenzofurans.
- Group I congeners have estrogenic activity and are potentially neurotoxic. They can activate hydroxylation reactions. They are metabolized more quickly than other PCB groups, with half-lives of several months.
- Group II congeners have dioxin-like properties. They are antiestrogenic by promoting the conversion of estradiol to the less active 2-hydroxy estradiol, likely due to their interaction with the aryl hydrocarbon receptor (AhR). They also affect metabolism of carcinogens via induction of cytochrome P450 enzymes. Half-lives range from 1-5 years.
- Group III congeners also induce cytochrome P450 enzymes and may be weakly estrogenic. However, they are much more persistent in the body than Group II congeners, as they are less amenable to metabolism. They also may enhance metabolism of carcinogens and conversion of estradiol to 16 alpha-hydroxyestrone (Wolff & Taniolo, 1995; Wolff et al., 1997). Half-lives may be greater than a decade.
Skin effects
Chloracne can be an overt sign of systemic exposure to PCBs, although its absence does not rule out exposure or the potential for other harmful effects. Chloracne has been reported in both acute and chronic PCB exposures. Exposure to dioxins and dibenzofurans is also associated with chloracne (Crow, 1970; Leijs et al., 2018; Letz, 1983; Maroni et al., 1981; Meigs et al., 1954).
- Distinctive features of chloracne include skin-colored cystic lesions that measure 1-10 mm, as well as open comedones (blackheads).
- Comedones and cysts may become inflamed and secondarily infected.
- Chloracne typically develops weeks or months after exposure and may occur at any age. Lesions most often appear on the chin, periorbital, and malar areas of the face, although the extremities and trunk may be affected as well.
- Skin lesions of chloracne may be resistant to treatment and can last for years or decades.
Hyperpigmentation may be a clinical indicator for moderate to high exposure to PCBs (Emmett et al., 1988).
Ocular effects.
- Workers exposed to airborne PCBs may develop eye irritation, tearing, or burning (Fischbein et al., 1985; Ouw et al., 1976; Smith et al., 1982).
- Meibomian gland hypersecretion, conjunctival pigmentation, and eyelid swelling have been observed in humans with occupational exposure to PCBs (Fu, 1984; Hsieh et al., 1996).
- Ocular effects tend to accompany chloracne (Fu 1984, Hsieh et al. 1996).
- Ocular findings may develop or persist after cessation of exposure, possibly due to dermal adipose accumulation of the causative (ATSDR, 2000).
Liver effects.
The liver is the main site of PCB metabolism. Metabolites are excreted in the bile and the urine. Persons with compromised hepatic function may potentially be more susceptible to adverse health effects from PCB exposure.
- PCB exposure is associated with increased levels of some liver enzymes, including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (AP), lactate dehydrogenase (LDH), and gamma-glutamyl transpeptidase (GGT) (ATSDR, 2000 & 2011; Maroni et al., 1981).
- Persons with hepatic involvement may experience nausea, vomiting, abdominal pain, anorexia, weight loss, jaundice, and uroporphyria (ATSDR, 2000).
- Asymptomatic liver enlargement has been reported in occupational exposures (Maroni et al., 1981).
- Ingestion of PCBs in food has been associated with increased incidence of chronic liver disease and cirrhosis (Hsieh et al., 1996).
- PCBs may induce hepatic microsomal enzymes, even after cessation of exposure. This may result in increased metabolism of certain therapeutic drugs, or otherwise cause disease resulting from increased metabolism of endogenous or exogenous substances (ATSDR, 2011).
Reproductive and developmental effects.
- Increased consumption of PCB-contaminated fish has been associated with higher relative risk of impaired reproductive ability in men but not women in one study (Courval et al., 1999).
- Men exposed to PCBs and polychlorinated dibenzofurans in-utero were found to have changes in semen quality, including abnormal morphology and reduced motility, although it is unknown if these findings are associated with fertility problems (Guo et al., 2000; Meeker & Hauser, 2010).
- Population-based studies suggest an inverse association between serum PCB and circulating testosterone levels in men and women (Meeker and Hauser, 2010).
- Developmental and neurobehavioral deficits have been observed in infants of mothers who ate moderate to high amounts of contaminated fish in the years prior to and during pregnancy. These deficits included weaker reflexes, immature motor function, and more-pronounced startle responses (Jacobson et al., 1984b; Swain, 1988). As a caveat, many of the epidemiologic studies on exposure to PCBs via fish consumption suffer from the confounding factor that fish contaminated with PCBs are often contaminated with other persistent organic pollutants, and in such situations, it is difficult to attribute clinical effects to a particular chemical.
- Neurodevelopmental delays such as impaired weight gain, poorer cognitive test performance, and lower verbal IQ scores have been reported in exposed children compared to controls (Aoki, 2001; Boucher et al., 2009; Ribas-Frito et al., 2001; Schantz et al., 2003).
Carcinogenicity.
The International Agency for Research on Cancer (IARC) has classified PCBs as carcinogenic to humans (IARC, 2016). The U.S. EPA has designated PCBs a probable human carcinogen. The Department of Health and Human Services concluded that PCBs are reasonably anticipated to be carcinogenic in humans based on sufficient evidence of carcinogenicity in animals (ATSDR, 2000 & 2011; Knerr & Schrenk, 2006).
- Exposure to PCBs appears to be associated with risk of malignant melanoma in some studies (IARC, 2016). Subsequent meta-analyses have yielded inconsistent findings (Boffetta et al., 2018; Zani et al., 2017).
- Non-Hodgkin lymphoma is also positively associated with PCB exposure, although results across high-quality studies were not always consistent (Engel et al., 2007; Zani et al., 2017).
- Breast cancer risk may be associated with PCB exposure, although results from high-quality studies have been heterogeneous. Some congeners are more strongly associated with the development of breast cancer than others (Leng et al. 2016, Zhang et al. 2015). Certain PCB congeners of groups II and III are positively associated with increased 5-year breast cancer-specific mortality, but not with longer-term breast cancer-specific mortality (Parada et al., 2020). Contaminants of commercial PCB products, such as dioxins, have also been found to have a positive association with breast cancer (VoPham et al., 2020).
- Sporadic positive and inconsistent findings were reported for gynecologic cancers, multiple myeloma, childhood acute lymphocytic leukemia, and cancers of the liver, biliary tract, brain, prostate, lung, thyroid, pancreas, colon/rectum, and stomach (ATSDR, 2000 & 2011; Bosetti et al., 2003; Faroon et al., 2001; IARC, 2016).
Endocrine and metabolic effects.
- Limited occupational studies suggest potential thyroid effects of PCB exposure including abnormal thyroid function, with some studies demonstrating an inverse association of triiodothyronine (T3) and thyroxine (T4) with PCBs (Salay & Garabrant, 2009).
- Increased odds ratio for goiter was found in a cohort with high exposure to PCBs and polychlorinated dibenzofurans (Guo et al., 1999).
- Multiple epidemiological studies have found positive associations between PCB exposure with insulin resistance, type 2 diabetes, obesity, and hypertension (Everett et al., 2011; Kim et al., 2019; Lee et al., 2006 & 2007a; Perkins et al., 2016).
- Among nondiabetics, there was a positive association between concentrations of nondioxin-like PCBs and a homeostasis model assessment of insulin resistance (Lee et al., 2007a).
- PCB concentrations were positively associated with waist circumference, as well as metabolic syndrome among nondiabetic participants in the CDC's National Health and Nutrition Examination Survey (NHANES) study (Lee et al., 2007b).
- PCBs may produce estrogenic or anti-estrogenic responses depending on the congener (Zhang et al., 2014).
Immune system effects.
- There is limited data to suggest that PCBs may cause immunosuppression and increased susceptibility to infections in children (Dallaire et al., 2006; Weisglas-Kuperus et al., 2004; Yu et al., 1998).
Clinical Evaluation
Patient History. A comprehensive occupational and environmental history emphasizing possible past and present exposures is essential when PCB exposure is suspected by either the patient or clinician. The initial interview should document the following patient information:
- Past medical history (including skin lesions, hepatitis or other liver disease, history of cancer, developmental history, gynecologic history)
- Current health signs and symptoms
- Skin lesions of chloracne and hyperpigmentation
- Ocular changes including irritation, tearing, burning, Meibomian gland hypersecretion, abnormal conjunctival pigmentation, and eyelid swelling
- Headache and dizziness
- Nausea, vomiting, abdominal pain, anorexia, weight loss, and jaundice
- Skin lesions of chloracne and hyperpigmentation
- Occupational exposure
- Any work involving manufacture of PCBs and PCB-containing products
- Repair, maintenance, or recycling of PCB-containing equipment
- Disposal of PCB-containing waste
- Working in old buildings with old caulk, paint, sealants, and other construction materials containing PCBs – with a specific route of exposure suspected
- Other occupations at high risk of exposure
- Source and intensity of exposure, if known
- Use of personal protective equipment
- When and for how long exposure or employment at that job occurred
- Any work involving manufacture of PCBs and PCB-containing products
- Dietary exposure
- Consumption of sport or game fish from PCB contaminated waters
- Consumption of sport or game fish from PCB contaminated waters
- Environmental exposure
- Exposure to material in hazardous waste sites that may contain PCBs
- Living or attending school in old buildings with old caulk, paint, sealants, and other construction materials containing PCBs – with a specific route of exposure suspected
- Living in the same household with someone who works in an occupation where they might be exposed to PCBs and introduce contamination into the home (Baker et al., 1980; Fischbein & Wolff, 1987).
- Hobbies that may result in possible exposure to PCBs, such as sportfishing and the use of PCB-containing materials such as old electronics and construction materials
- Exposure to material in hazardous waste sites that may contain PCBs
Physical Examination. When performing the physical exam, focus on the major organs and systems that PCB exposure may affect, including the following:
- Skin
- Thyroid
- Heart and lungs
- Breasts
- Liver
- Nervous system
Tests and Imaging
Diagnostic Tests. The decision to perform additional tests should be based on the patient's history and clinical evaluation, weighing possible risks and benefits of additional testing.
Elevation of serum liver enzymes including aspartate transaminase (AST), alanine transaminase (ALT), gamma-glutamyl transpeptidase (GGT), lactate dehydrogenase (LDH), alkaline phosphatase (AP), and bilirubin have been observed, but these tests are neither sensitive nor specific for detection of PCB exposure.
Serum PCB level testing is available, but the results are often difficult to interpret. NHANES data provides congener-specific PCB levels in the general U.S. population from a national sample (CDC, 2022; Lee et al., 2007b). Testing may be considered to confirm history of high-dose acute or chronic exposure but is unlikely to affect clinical management decisions. No known consistent causal associations exist between serum levels and specific adverse health effects.
Consider the following diagnostic tests for evaluation of a PCB-exposed patient:
- Baseline serum liver enzymes
- Perform subsequent liver enzyme testing only if indicated for patients with known history of extensive exposure (e.g. accidental spill or occupational exposure) or with potential for ongoing occupational or environmental exposure.
- In patients with elevated liver enzymes, rule out other causes of liver disease including alcohol ingestion, non-alcoholic fatty liver disease, infectious hepatitis, infiltrative processes, connective tissue diseases, and rare genetic conditions.
- Perform subsequent liver enzyme testing only if indicated for patients with known history of extensive exposure (e.g. accidental spill or occupational exposure) or with potential for ongoing occupational or environmental exposure.
- Skin biopsy may confirm chloracne.
- Serum PCB level may be considered for persons with signs and symptoms suggestive of high levels of exposure (e.g., chloracne, elevated liver enzymes) to confirm exposure.
Radiographic imaging. No specific imaging modality is indicated for routine evaluation of known or potential PCB exposure in asymptomatic patients. In patients with signs and symptoms of liver involvement, abdominal ultrasound may be helpful.
Treatment and Patient Management
PCB exposure has no specific antidote. Treatment is primarily supportive.
It is important to remove the patient from the exposure source to stop ongoing exposure.
Acute exposure:
- For acute skin and eye exposure, flush immediately with copious amounts of water.
- Remove contaminated clothing and discard properly.
- Observe patients with inhalational exposure for systemic symptoms and treat as necessary, although no specific measures are available to reduce PCB absorption via the respiratory tract.
- In the rare event of acute PCB ingestion, do not induce vomiting, which may cause aspiration of stomach contents into the respiratory tract. The efficacy of administering activated charcoal is unknown.
Chronic exposure:
- Initial treatment of chloracne is based on cessation of PCB exposure and good skin hygiene.
- Chloracne may be highly resistant to treatment. Occasionally, antibiotics may be indicated for secondary bacterial infection. Consider referral to dermatology for assistance in developing a treatment plan.
- No prophylactic medication or treatment is currently available to prevent the development or progression of PCB-related health effects associated with chronic exposure.
Patient Follow-Up
Patients who have been exposed to PCBs may need close outpatient follow-up.
- Periodic clinical evaluations may detect abnormalities at an early stage, if they occur. Further testing may be performed based on symptoms, physical exam findings, and standard clinical practice.
- There are no authoritative recommendations for screening tests to detect health outcomes related to PCB exposure. General screening for cancer and other chronic diseases should be done in accordance with the recommendations of the U.S. Preventive Services Task Force (USPSTF) based on the patient's age, sex, and other risk factors (USPSTF, 2017).
- Consider consultation with a specialist in occupational and environmental medicine or other clinician with the expertise and experience for treating and managing patients exposed or potentially exposed to PCBs and who can assist with development of a periodic monitoring plan, as appropriate.
Patient Counseling and Exposure Reduction
- Encourage the use of administrative controls such as reducing exposure time for employees, work practice controls including appropriate hygiene when working in areas containing PCBs, and appropriate personal protective equipment when working with materials known to contain PCBs. Advise caution when working with old electrical equipment that may be damaged.
- Recommend avoiding physical contact with potentially contaminated materials like soil. Advise parents/guardians to prevent children from playing near hazardous waste sites; in addition to other potential hazards, PCBs may contaminate the surrounding soil, which could lead to oral ingestion from hand-to-mouth activity and to dermal uptake.
- Encourage patients to check local, state, tribal, and federal fish consumption advisories where they fish.
- Fish consumption during pregnancy is recommended, as fish provide many nutrients important for development. However, there are important considerations for people who are or plan to become pregnant because of the increased prevalence of developmental and neurobehavioral deficits in infants born to mothers who consume higher amounts of PCB-contaminated fish.
- The U.S. Food & Drug Administration (FDA) and EPA publish advice about eating fish for people who are or might become pregnant (EPA, 2021; FDA, 2021).
- People who are or might become pregnant should be encouraged to choose "best choices" from the FDA/EPA species lists, varying their fish sources, and choosing short-lived fish low on the food chain such as salmon (USPSTF, 2017). Following these guidelines allows for the benefits of fish consumption while minimizing the risk from PCBs or other contaminants in some fish.
- The U.S. Food & Drug Administration (FDA) and EPA publish advice about eating fish for people who are or might become pregnant (EPA, 2021; FDA, 2021).
Other Sources of Information on PCBs
Additional Resources
- Toxicological Profile for Polychlorinated Biphenyls (PCBs), Agency for Toxic Substances and Disease Registry (ATSDR)
- Tox FAQs for Polychlorinated Biphenyls (PCBs), Agency for Toxic Substances and Disease Registry (ATSDR) - These FAQ can be used for patient education.
- Advice about Eating Fish
- Polychlorinated Biphenyls (PCBs), Environmental Protection Agency (EPA)
Clinical Resources
- Taking an Exposure History
- Pediatric Environmental Health Specialty Units (PEHSU) - A network of experts in reproductive and children's environmental health.
- Association of Occupational and Environmental Clinics (AOEC)
- American Association of Poison Control Centers (AAPCC)
- ATSDR Case Studies in Environmental Medicine:
- Biomonitoring Data Tables for Environmental Chemicals, National Health and Nutrition Examination Survey (NHANES)
Contact Us
For more information about these products, email ATSDR's Environmental Medicine and Health Systems Intervention Section at envmed@cdc.gov.
For questions or information on other products and topics, contact CDC–INFO.
- (AAP) American Academy of Pediatrics, Council on Environmental Health. (2019). Breast milk. InR Etzel, (Ed), Pediatric environmental health, 237 - 257. (4th Ed.).
- Ando M, Saito H, & Wakisaka I. (1985). Transfer of polychlorinated biphenyls (PCBs) to newborn infants through the placenta and mothers' milk. Archives of Environmental Contamination and Toxicology, 14(1), 51-57. https://pubmed.ncbi.nlm.nih.gov/3919656/
- Aoki Y. (2001). Polychlorinated biphenyls, polychlorinated dibenzo-p-dioxins, and polychlorinated dibenzofurans as endocrine disrupters: What we have learned from Yusho disease. Environmental Research, 86(1), 2-11. https://pubmed.ncbi.nlm.nih.gov/11386736/
- (ATSDR) Agency for Toxic Substances and Disease Registry. (2000). Toxicological profile for polychlorinated biphenyls (PCBs). (ATSDR) Agency for Toxic Substances and Disease Registry. (2011). Addendum to the toxicological profile for polychlorinated biphenyls. https://www.atsdr.cdc.gov/toxprofiles/pcbs_addendum.pdf
- (ATSDR) Agency for Toxic Substances and Disease Registry. 2011. Addendum to the Toxicological Profile for Polychlorinated Biphenyls. (Accessed Oct. 20, 2023) https://www.atsdr.cdc.gov/toxprofiles/pcbs_addendum.pdf
- (ATSDR) Agency for Toxic Substances and Disease Registry. (2021). PFAS and breastfeeding. https://www.atsdr.cdc.gov/pfas/docs/pfas-breastfeeding-h.pdf
- Baker Jr EL, Landrigan PJ, Glueck CJ, Zack Jr MM, Liddle JA, Burse VW, Housworth WJ, & Needham LL. (1980). Metabolic consequences of exposure to polychlorinated biphenyls (PCB) in sewage sludge. American Journal of Epidemiology, 112(4), 553-63. https://pubmed.ncbi.nlm.nih.gov/6775528/
- Boffetta P, Catalani S, Tomasi C, Pira E, & Apostoli P. (2018). Occupational exposure to polychlorinated biphenyls and risk of cutaneous melanoma: a meta-analysis. European Journal of Cancer Prevention, 27(1), 62-69. https://pubmed.ncbi.nlm.nih.gov/27749494/
- Bosetti C, Negri E, Fattore E, & La Vecchia C. (2003). Occupational exposure to polychlorinated biphenyls and cancer risk. European Journal of Cancer Prevention, 12(4), 251-255. https://pubmed.ncbi.nlm.nih.gov/12883375/
- Boucher O, Muckle G, & Bastien CH. (2009). Prenatal exposure to polychlorinated biphenyls: a neuropsychologic analysis. Environmental Health Perspectives ,117(1), 7-16. https://pubmed.ncbi.nlm.nih.gov/19165381/
- (CDC) Centers for Disease Control and Prevention. (2022). National report on human exposure to environmental chemicals biomonitoring data tables for environmental chemicals. https://www.cdc.gov/exposurereport/data_tables.html
- Courval JM, DeHoog JV, Stein AD, Tay EM, He J, Humphrey HE, & Paneth N. (1999). Sport-caught fish consumption and conception delay in licensed Michigan anglers. Environmental Research, 80(2 Pt 2), S183-S188. https://pubmed.ncbi.nlm.nih.gov/10092432/
- Crow KD. (1970). Chloracne. British Journal of Dermatology, 83(5), 599-600
- Dai Q, Min X, & Weng M. (2016). A review of polychlorinated biphenyls (PCBs) pollution in indoor air environment. Journal of the Air & Waste Management Association, 66(10), 941-950. https://pubmed.ncbi.nlm.nih.gov/27191511/
- Dallaire F, Dewailly E, Vézina C, Muckle G, Weber JP, Bruneau S, & Ayotte P. (2006). Effect of prenatal exposure to polychlorinated biphenyls on incidence of acute respiratory infections in preschool Inuit children. Environmental Health Perspectives, 114(8), 1301-1305. https://pubmed.ncbi.nlm.nih.gov/16882544/
- Emmett EA, Maroni M, Schmith JM, Levin BK, & Jefferys J. (1988). Studies of transformer repair workers exposed to PCBs: I. Study design, PCB concentrations, questionnaire, and clinical examination results. American Journal of Industrial Medicine, 13(4), 415-427. https://pubmed.ncbi.nlm.nih.gov/3129934/
- Engel LS, Lan Q, and Rothman N. (2007). Polychlorinated biphenyls and non-Hodgkin lymphoma. Cancer Epidemiology, Biomarkers & Prevention, 16(3), 373-376.
- (EPA) U.S. Environmental Protection Agency. (2021). EPA-FDA advice about eating fish and shellfish. https://www.epa.gov/choose-fish-and-shellfish-wisely/epa-fda-advice-about-eating-fish-and-shellfish
- Everett CJ, Frithsen I, & Player M. (2011). Relationship of polychlorinated biphenyls with type 2 diabetes and hypertension. Journal of Environmental Monitoring, 13(2), 241-251. https://pubmed.ncbi.nlm.nih.gov/21127808/
- Faroon OM, Keith S, Jones D, & De Rosa C. (2001). Carcinogenic effects of polychlorinated biphenyls. Toxicology and Industrial Health, 17(2), 41-62. https://pubmed.ncbi.nlm.nih.gov/12117297/
- (FDA) U.S. Food & Drug Administration. (2021). Advice about eating fish for those who might become or are pregnant or breastfeeding and children ages 1-11 years. https://www.fda.gov/food/consumers/advice-about-eating-fish#choice
- Fischbein A, Rizzo JN, Solomon SJ, & Wolff MS. (1985). Oculodermatological findings in workers with occupational exposure to polychlorinated biphenyls (PCBs). British Journal of Industrial Medicine, 42(6), 426-430. https://pubmed.ncbi.nlm.nih.gov/3924093/
- Fischbein A & Wolff MS. (1987). Conjugal exposure to polychlorinated biphenyls (PCBs). British Journal of Industrial Medicine, 44(4), 284-286. https://pubmed.ncbi.nlm.nih.gov/3105572/
- Fu YA. (1984). Ocular manifestation of polychlorinated biphenyls intoxication. American Journal of Industrial Medicine, 5(1-2), 127-132. https://pubmed.ncbi.nlm.nih.gov/6422743/
- Gouin, T, Mackay D, Jones KC, Harner T, & Meijer SN. (2004). Evidence for the "grasshopper" effect and fractionation during long-range atmospheric transport of organic contaminants. Environmental Pollution, 128(1-2), 139-148. https://pubmed.ncbi.nlm.nih.gov/14667724/
- Grimm FA, Hu D, Kania-Korwel I, Lehmler HJ, Ludewig G, Hornbuckle KC, Duffel MW, Bergman Å, & Robertson LW. (2015). Metabolism and metabolites of polychlorinated biphenyls. Critical Reviews in Toxicology, 45(3), 245-272. https://pubmed.ncbi.nlm.nih.gov/25629923/
- Guo YL, Yu ML, Hsu CC, & Rogan WJ. (1999). Chloracne, goiter, arthritis, and anemia after polychlorinated biphenyl poisoning: 14-year follow-up of the Taiwan Yucheng cohort. Environmental Health Perspectives, 107(9), 715-719. https://pubmed.ncbi.nlm.nih.gov/10464071/
- Guo YL, Hsu PC, Hsu CC, & Lambert GH. (2000). Semen quality after prenatal exposure to polychlorinated biphenyls and dibenzofurans. The Lancet, 356(9237), 1240-1241. https://pubmed.ncbi.nlm.nih.gov/11072947/
- Hansen LG. (1987). Environmental toxicology of polychlorinated biphenyls. In S Safe S (Ed.) Polychlorinated biphenyls (PCBs): Mammalian and environmental toxicology. Environmental toxin series (1st ed., pp. 15-48), Springer Publishing.
- Hansen LG. (1999). The ortho side of PCBs: Occurrence and disposition. Kluwer Academic Publishers.
- Hsieh SF, Yen YY, Lan SJ, Hsieh CC, Lee CH, & Ko YC. (1996). A cohort study on mortality and exposure to polychlorinated biphenyls. Archives of Environmental Health, 51(6), 417-424. https://pubmed.ncbi.nlm.nih.gov/9012319/
- Humphrey HEB. (1983). Population studies of PCBs in Michigan residents. In: FM D'Itri and MA Kamrin, (Eds.), PCBs:Human and environmental hazards (pp. 299-310), Butterworth-Heinemann Elsevier Ltd.
- (IARC) International Agency for Research on Cancer. (2016). Polychlorinated biphenyls and polybrominated biphenyls. IARC Monographs on the Evaluation of the Carcinogenic Risks of Chemicals to Humans, 107, 9-500.
- Jacobson JL, Fein GG, Jacobson SW, Schwartz PM, & Dowler JK. (1984a). The transfer of polychlorinated biphenyls (PCBs) and polybrominated biphenyls (PBBs) across the human placenta and into maternal milk. American Journal of Public Health, 74(4), 378-379. https://pubmed.ncbi.nlm.nih.gov/6322600/
- Jacobson JL, Jacobson SW, Schwartz PM, Fein GG, & Dowler JK. (1984b). Prenatal exposure to environmental toxin: A test of the multiple effects model. Developmental Psychology, 20(4), 523-532.
- Kim YA, Park JB, Woo MS, Lee SY, Kim HY, and Yoo YH. (2019). Persistent organic pollutant-mediated insulin resistance. International Journal of Environmental Research and Public Health, 16(3), 448. https://pubmed.ncbi.nlm.nih.gov/30717446/
- Knerr S & Schrenk D. (2006). Carcinogenicity of "non-dioxinlike" polychlorinated biphenyls. Critical Reviews in Toxicology, 36(9), 663-694. https://pubmed.ncbi.nlm.nih.gov/17050081/
- Lee DH, Lee IK, Song K, Steffes M, Toscano W, Baker BA, & Jacobs Jr DR. (2006). A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the national health and examination survey 1999-2002. Diabetes Care, 29(7), 1638-1644. https://pubmed.ncbi.nlm.nih.gov/16801591/
- Lee DH, Lee IK, Jin SH, Steffes M, & Jacobs Jr DR. (2007a). Association between serum concentrations of persistent organic pollutants and insulin resistance among nondiabetic adults: results from the national health and nutrition examination survey 1999-2002. Diabetes Care, 30(3), 622-628. https://pubmed.ncbi.nlm.nih.gov/17327331/
- Lee DH, Lee IK, Porta M, Steffes M, & Jacobs Jr DR. (2007b). Relationship between serum concentrations of persistent organic pollutants and the prevalence of metabolic syndrome among non-diabetic adults: results from the National Health and Nutrition Examination Survey 1999–2002. Diabetalogia, 50(9), 1841-1851. https://pubmed.ncbi.nlm.nih.gov/17624515/
- Leijs MM, Esser A, Amann PM, Schettgen T, Gube M, Merk HF, Kraus T, & Baron JM. (2018). Hyperpigmentation and higher incidence of cutaneous malignancies in moderate-high PCB- and dioxin exposed individuals. Environmental Research, 164, 221-228. https://pubmed.ncbi.nlm.nih.gov/29501832/
- Letz G. (1983). The toxicology of PCB's–an overview for clinicians. The Western Journal of Medicine, 138(4), 534-540. https://pubmed.ncbi.nlm.nih.gov/6223449/
- Maroni M, Colombi A, Arbosti G, Cantoni S, & Foa V. (1981). Occupational exposure to polychlorinated biphenyls in electrical workers. II. health effects. British Journal of Industrial Medicine, 38(1), 55-60. https://pubmed.ncbi.nlm.nih.gov/6451237/
- Maroni M, Colombi A, Arbosti G, Cantoni S, & Foa V. (1981). Occupational exposure to polychlorinated biphenyls in electrical workers. II. health effects. British Journal of Industrial Medicine, 38(1), 55-60. https://pubmed.ncbi.nlm.nih.gov/6451237/
- McLachlan M. (1993). Digestive tract absorption of polychlorinated dibenzo-p-dioxins, dibenzofurans, and biphenyls in a nursing infant. Toxicology and Applied Pharmacology, 123(1), 68-72. https://pubmed.ncbi.nlm.nih.gov/8236263/
- Meeker JD & Hauser R. (2010). Exposure to polychlorinated biphenyls (PCBs) and male reproduction. Systems Biology in Reproductive Medicine, 56(2), 122-131. https://pubmed.ncbi.nlm.nih.gov/20377311/
- Meigs JW, Albom JW, & Kartin BL. (1954). Chloracne from an unusual exposure to arochlor. Journal of the American Medical Association, 154(17), 1417-1418. https://pubmed.ncbi.nlm.nih.gov/13151867/
- Ouw HK, Simpson GR, & Siyali DS. (1976). Use and health effects of aroclor 1242, a polychlorinated biphenyl, in an electrical industry. Archives of Environmental Health, 31(4), 189-194. https://pubmed.ncbi.nlm.nih.gov/821401/
- Parada H, Sun X, Tse CK, Engel LS, Hoh E, Olshan AF, & Troester MA. (2020). Plasma levels of polychlorinated biphenyls (PCBs) and breast cancer mortality: The Carolina Breast Cancer Study. International Journal of Hygiene and Environmental Health, 227, 113522. https://pubmed.ncbi.nlm.nih.gov/32276222/
- Perkins JT, Petriello MC, Newsome BJ, & Hennig B. (2016). Polychlorinated biphenyls and links to cardiovascular disease. Environmental Science and Pollution Research International, 23(3), 2160-2172. https://pubmed.ncbi.nlm.nih.gov/25877901/
- Ribas-Fito N, Sala M, Kogevinas M, & Sunyer J. (2001). Polychlorinated biphenyls (PCBs) and neurological development in children: a systematic review. Journal of Epidemiology and Community Health, 55(8), 537-546. https://pubmed.ncbi.nlm.nih.gov/11449010/
- Salay E, Garabrant D. (2009). Polychlorinated biphenyls and thyroid hormones in adults: a systematic review appraisal of epidemiological studies. Chemosphere, 74(11), 1413-1419. https://pubmed.ncbi.nlm.nih.gov/19108870/
- Schantz SL, Jacobson JL, Humphrey HEB, Jacobson SW, Welch R, & Gasior D. (1994). Determinants of polychlorinated biphenyls (PCBs) in the sera of mothers and children from Michigan farms with PCB-contaminated silos. Archives of Environmental Health, 49(6), 452-458. https://pubmed.ncbi.nlm.nih.gov/7818287/
- Schantz SL, Widholm JJ, & Rice DC. (2003). Effects of PCB exposure on neuropsychological function in children. Environmental Health Perspectives, 111(3), 357-576. https://pubmed.ncbi.nlm.nih.gov/12611666/
- Smith AB, Schloemer J, Lowry LK, Smallwood AW, Ligo RN, Tanaka S, Stringer W, Jones M, Hervin R, & Glueck CJ. (1982). Metabolic and health consequences of occupational exposure to polychlorinated biphenyls. British Journal of Industrial Medicine, 39(4), 361-369. https://pubmed.ncbi.nlm.nih.gov/6128023/
- Swain WR. (1998). Human health consequences of consumption of fish contaminated with organochlorine compounds. Aquatic Toxicology, 11(3), 357-377.
- (USPSTF) U.S. Preventive Services Task Force. (2017). Recommendations. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics
- VoPham T, Bertrand KA, Jones RR, Deziel NC, DuPré NC, James P, Liu Y, Vieira VM, Tamimi RM, Hart JE, Ward MH, & Laden F. (2020). Dioxin exposure and breast cancer risk in a prospective cohort study. Environmental Research, 186, 109516. https://pubmed.ncbi.nlm.nih.gov/32305677/
- Wania F & Mackay D. (1996). Tracking the distribution of persistent organic pollutants. Environmental Science & Technology, 30(9), 390A-396A. https://pubmed.ncbi.nlm.nih.gov/21649427/
- Weisglas-Kuperus N, Vreugdenhil HJI, & Mulder PGH. (2004). Immunological effects of environmental exposure to polychlorinated biphenyls and dioxins in Dutch school children. Toxicology Letters, 149(1), 281-285. https://pubmed.ncbi.nlm.nih.gov/15093274/
- Wolff MS & Toniolo PG. (1995). Environmental organochlorine exposure as a potential etiologic factor in breast cancer. Environmental Health Perspectives, 103(Suppl 7), 141-145. https://pubmed.ncbi.nlm.nih.gov/8593861/
- Wolff MS, Camann D, Gammon M, & Stellman SD. (1997). Proposed PCB congener groupings for epidemiological studies. Environmental Health Perspectives, 105(1), 13-14. https://pubmed.ncbi.nlm.nih.gov/9074863/
- Yu ML, Hsin JW, Hsu CC, Chan WC, & Guo YL. (1998). The immunologic evaluation of the Yucheng children. Chemosphere, 37(9-12), 1855-1865. https://pubmed.ncbi.nlm.nih.gov/9828314/
- Zani C, Ceretti E, Covolo L, & Donato F. (2017). Do polychlorinated biphenyls cause cancer? A systematic review and meta-analysis of epidemiological studies on risk of cutaneous melanoma and non-Hodgkin lymphoma. Chemosphere, 183, 97-106. https://pubmed.ncbi.nlm.nih.gov/28535466/
- Zhang J, Huang Y, Wang X, Lin K, & Wu K. (2015). Environmental polychlorinated biphenyl exposure and breast cancer risk: a meta-analysis of observational studies. PLOS ONE,10(11), e0142513. https://pubmed.ncbi.nlm.nih.gov/26555153/
- CDC. (No date). No title [photograph]. CDC. https://www.cdc.gov/niosh/topics/skin/occderm-slides/ocderm5.html
- Cade Martin. (2009). No title [photograph]. CDC/Dawn Arlotta. https://phil.cdc.gov/Details.aspx?pid=11336

